At 14 years of age, Al felt triumphant as he announced his transgender male identity publicly. His social transition had been successful, and he was no longer known as Alice. But, his exuberance did not last long. Al soon became ready to move forward in his gender transition with the use of medical interventions, but was met with obstacles out of his control. Our state laws do not allow such a young person access to medical interventions without parental consent. Al’s mom was just beginning to get used to the idea of having a son, not a daughter, and was not prepared to support hormone blockers—a next step in his transition. A transgender youth in our state must be 15 years old to consent to this treatment. Our therapeutic task included helping Al emotionally manage the discrepancies between what he desired and the legal realities he faced.
As may be apparent from the beginning of this story, Al demonstrated a high level of maturity and capacity for insight for his chronological age. He routinely researched transgender stories and options and was willing to educate both me and his mother. But, proclaiming his male self to himself, and to society did not relieve Al’s inner turmoil nor decrease symptoms of his Generalized Anxiety Disorder (GAD). One indication of his fluctuating sense-of-self was that he changed his name at least four times during the course of his treatment. Another was that, as our sessions proceeded, Al’s distress with the incongruence between his sense of himself and his developing female body left him constantly exasperated.
When Al’s breasts began to develop more rapidly, he was forced to confront his dysphoria daily. His anxiety soared. His self-loathing increased as he became “more curvy” and had to deal with menstrual periods and his “female voice.” Increasingly, these bodily functions fueled his frustration, sense of hopelessness, and self-hate. His Gender Dysphoria (GD) became extreme. Al became more anxious and despondent. His self-talk was filled with anxiety-driven disparaging messages like, “I’m bad, worthless, and the world would be better off without me.” He began to reveal more frequent thoughts of suicide stating, “I don’t deserve to be here!” Al felt betrayed by his own body and groaned, “I can’t stand the thought of growing up into a woman!” He became more depressed as he objectified his body and treated it as the hated other. When using binders to fit in socially, they did not decrease his daily aversion to his own body that he had to see each day. Using binders also risked pain and had the potential for other physical problems.
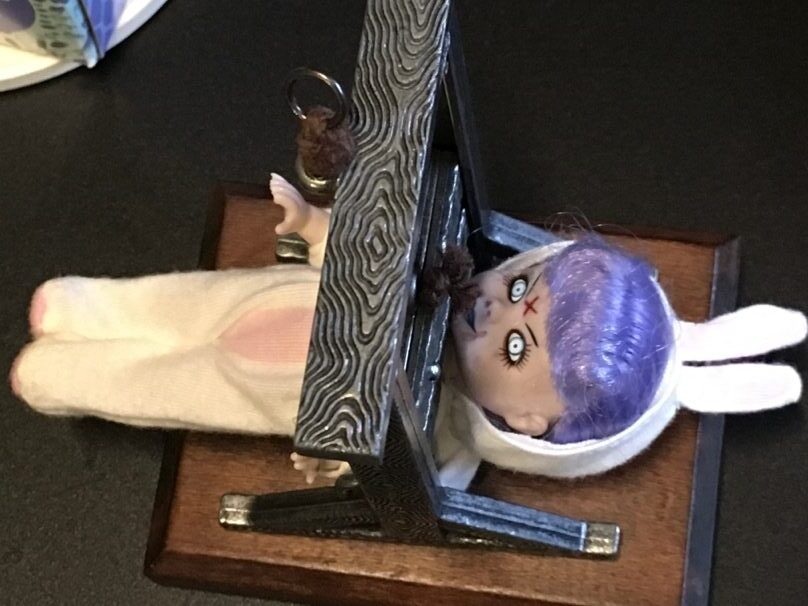

Al’s dysphoria formed emotional whirlwinds that evoked his patterns of negative anxiety thoughts, and he felt the need to imagine his dysphoria. The figure of the “evil bunny girl” that he used previously, again appeared often (Figure 1). The day he found the guillotine and played with cutting off her head he stated, “This feels good.” Another visualization of his dysphoria started with the female doll form placed alone in the center of the sand tray (Figure 2). After seeing a play that had characters feigning nudity, Al reported that his dysphoria was “up front”—that he became envious and frustrated when the men took off their shirts. The next day he was misgendered and called his “dead name,” Alice, at a medical visit. As this sand world progressed he placed supportive items such as Buddhas (“spirituality”), food (“care of my body”), and a grouping of “male power figures” (southwest corner in figure 4). Al eventually placed the “evil bunny girl” of dysphoria on the top of the doll form (Figure 3). He revealed that she evoked a feeling of self-disgust. Al set the smaller male and female miniatures separating them across the tray, sharing, “I know I’m not going to change back to a woman” (Figure 4). He stated that the items on the south side of the tray helped him deal with seeing the dysphoria. At the end Al asked to guillotine the bunny again, and did so.


Al’s anxiety disorder and his gender dysphoria interfered with his concentration, moods, and sleep with a negative impact on his focus at school. He was always an advanced student, but began to struggle with his academic performance. He developed a Panic Disorder. His irritability impacted all of his relationships and he struggled daily to dress and prepare for school. He spent much time fixing his hair and clothes to disguise the reality of his female body. Al had difficulty looking in the mirror which never reflected his felt self. His appearance often became fuel for his negative and circular anxiety patterns. Al and I named these swirling thoughts his “anxiety squirrels.” This pattern of “anxiety squirrels” could hijack any thought or feeling and overwhelm him. His frustration grew and in anger he affirmed, “My body is doing things against my will!” Buying clothes that he felt good in became a challenge and then, when he moved from boy’s clothes to men’s, a nightmare. His hips widened, and clothes did not fit well. He was concerned about what bathroom to use; although at school he was offered the use of the staff bathrooms, in reality these were often inaccessible. On overnight school trips, sleeping/roommate arrangements were an issue requiring negotiations including those for Al’s safety. His life was consumed by his sense of being in a wrong body.
As his female body advanced further into puberty, I became alarmed at the deterioration of Al’s mental health. His rage that he was not born in a male body turned inward— “I was born with the tools of a woman, but that’s not me!” Although Al did not report a specific suicide plan, I was aware of the high rate of suicide in transgender youth. Al eventually admitted to cutting and we had to negotiate a safe place, out of his house, for his sharps, while he developed other coping skills. Al and his family did not believe in using “Big Pharma,” and so they rejected my suggestion for a medication review in favor of homeopathy, Chinese herbs, CBD, and other non-pharmaceutical approaches. Each worked for a time, but when his panic episodes became unmanageable by any other means, Al required conventional medication.
After decades of keeping a hard boundary between my office and private time, when I observed Al’s rapid deterioration due to his anxiety disorder, I recognized the need for a change. In response to his impulsivity to self-harm, I allowed him to make needed urgent contacts with me between sessions. His distress lessened when I could “nip it in the bud” in a timely manner by challenging his cognitive distortions and helping him reset his physical and mental focus. These short interventions helped grow his capacity for emotional regulation, in turn insuring that he was more able to work in his regular therapy sessions. When I could not be readily available, I provided him a specific time for a phone call which eased his escalation. Eventually, Al was able to use the Trevor Project hot line for his urgent care needs.
In our state a youth must be 15 years old to determine their own use of hormone blockers. The problem was that Al’s onset of puberty came early and proceeded rapidly. He not only met the common markers of “persistent and consistent” about being a trans male, he became a strong advocate for himself and his desire for hormone blockers long before the legal age allowed. “The longer I wait the curvier I get….I need to get Alice out of the way.”
Trans care was a regular area of conflict between Al and his mom. Al’s mom initially was against any medical interventions for transgender care. She could not accept that he knew that he was a male, and would not change his mind. I encouraged Mom to begin her learning by viewing a PBS documentary on transgender kids and their families. I also facilitated a referral for the family to a major medical center providing transgender care. I’d hoped that Mom could find support associating with other parents struggling with their children’s’ GD. Mom also learned there that youth who begin their trans journey in their teens are highly unlikely to change their minds.
Eventually I asserted that from a mental health standpoint Al needed hormone blockers as, the more time passed, the more he demonstrated greater body aversion and self-hate—“The world sucks and I want to die!” The mental health costs to Al if he had to wait another 6 to12 months for gender affirming care would only increase. In advocating for Al’s medical care with his mom, I paraphrased a parent’s reflection reported in the literature. That parent was in the ER with a trans child who had nearly succeeded in their suicide attempt. I asked Al’s mom if she would rather have a live son than a dead daughter, because that was a real risk. With further education Mom changed her mind to allow hormone blockers (HB). She made it clear that blockers were as far as she would go until Al became of legal age to choose for himself. These puberty blockers prevent the continuation of sexual maturation. They do not create the lifelong infertility, and are not permanent as with cross-sex hormones, such a testosterone (T) which Al also desired.
Even with his mother’s support, getting hormone blockers for Al required effort. His medical provider didn’t have previous experience prescribing for so young a teen. We engaged in several conversations, and she requested a letter from me in support of this treatment. Al’s persistent and consistent presentation that he felt male, and his deteriorating mental health with the advancement of his puberty in female body, were well documented. It is important to note that the DSM5 criteria for Gender Dysphoria in Adolescents and Adults includes six points for criteria A. Only two are required to make this diagnosis. Al met all six markers. Criteria B is related to personal distress and social impairment. Al’s distress was palpable and his social functioning had declined.
Hormone blockers do not make an immediate observable impact. Al had the knowledge that his breasts would stop growing, his periods would stop, and his trans care trajectory was going in the right direction. He expressed some relief and felt a bit more supported by his mom. Al’s expressive artwork revealed an intermittent budding hope. After taking blockers for 10 months, Al spontaneously said, “I actively want to live now.” His body betrayed him less and he demonstrated greater interest in life. Al’s negative anxiety patterns did not dissolve and required continuous therapeutic intervention. At his worst, any dysphoric feeling would activate his “anxiety squirrel” pattern and he could spiral into despair. His dysphoria was reduced and eventually did not automatically trigger self-harm impulses. The struggle for Al between supporting himself and fueling his self-hate remained. He also realized that he had entered a long term relationship with the medical establishment that he’d feared since his father’s illness and death.


In one session, Al created a sand world of a maze (Figures 6 & 7). “It appears to be a place where all one’s needs are met, but is really a trap. The center appears to be a happy place in the midst of chaos-but it’s a cage. It’s too good to be true.” That day, a time of increased dysphoria, he felt that this creation reflected his inner chaos. He used this image, a shared language between us, multiple times over the years. At one time it depicted the maze of the medical establishment and all of his choices.
When he became 16 years old, the legal age for this request, Al sought testosterone treatment (T). He expressed anxiety over giving himself injections, but he never wavered in his desire for the results T would bring. Despite the use of a voice coach, his “girl voice” could easily trigger his gender dysphoria which would evoke the “anxiety squirrels.” Al wanted a male appearing and sounding body and knew this treatment would get him closer to presenting his authentic self to the world. Within a month of starting T, Al’s art depicted an increase in themes of nurturing, growth, and community. He continued to struggle with his anxiety and dysphoria, but the intensity of his self-deprecations decreased in frequency. Then, just prior to the Covid pandemic, Al lost a close family member who lived with him. His grief became a focus of care for months as his functioning again declined.
Covid’s isolation brought Al freedom from the societal pressures about being transgender. Yet the threat from the Covid virus escalated his anxiety and reduced his capacity to self-manage his thoughts and feelings. Like many students he struggled with the adjustment to online school and lost physical contact with his group of supportive friends. Al’s therapy also went to video. By then we had worked together long enough that video sessions were adequate. Al was continuing with his T shots and noticed his body changing. He petitioned the court to change his name and birth certificate to reflect his male identity. Using poetry, collage, drawing, and Al’s journal entries we preceded to work on his grief, anxiety, and gender issues. His overuse of electronic devices and their function in his anxiety system also became a treatment issue.
After the Covid shutdown, Al was eager to return to school. The therapeutic work on his body image and identity continued. His anxiety and gender difficulties remained a focus but the immediate threat to his life diminished. He struggled to be “a real man.” His normal maturation aided his ability to both engage in treatment and to self-manage, but he struggled with consistent self-care. Al’s GD symptoms improved with the changes to his body, including his voice. At one point he shared, “Hope is a very scary thing to have.” Al’s anxiety remained notable but he gained more confidence and engaged in several extracurricular activities. His increased self-acceptance helped Al recognized that his capacity to love is not in the other person, but in himself. Al’s path was not linear or smooth, but he grew stronger.
Al later graduated from high school with a four-year college scholarship. He had been considering top surgery for some time. This procedure would contour his chest to reflect his male identity, so he delayed college entry for a year. As his male identity strengthened he no longer eschewed the feminine aspects, and stated, “The more I am able to embrace my female energy, the more masculine I get.” After high school graduation he held a ritualized funeral for himself stating, “this is for the death of an imagined future, not for my past self.” He planned to bury a “casket” in the forest, so we worked on creating items for this event. On the day of the burial he awoke with the awareness, “I am someone who is loved.” Subsequently, he held a “Rebirthday Party” with his closest friends. Eventually Al’s panics declined, controlled by a combination of prescription medication with a homeopathic remedy. Several months after high school graduation Al had his top surgery, fully cared for and supported by his mother.
Al got a job and needed to come to treatment less often. We continued our work adding preparations for him to move to college and find a new therapist. As he was preparing to move out of state, Al came in and created his last sand world which we continued to process into the next session as well.

Al created separate areas in his sand tray reflecting aspects of himself (Figure 8). He worked and reworked the boundaries and what formed them. The horizontal “river” is the main border. “What is south of the river [closest to him] is what I know and project to the outside” (persona). What is north of the river [opposite to him] is “what I see but is unknown.” We explored how he cultivates his persona and sees his internal and external selves. The center north segment holds the “spiritual energies” for Al. “Now I am more in agreement with my body, so it’s more of a spiritual question than an action item.” The area to the east with the owl is a “childhood with pain” (Figure 9). The upside down mirror is the lack of reflection of his true self. Noting the owl, “I feel like a Russian nesting doll.” Al described feeling like he has layers on top of layers of himself. “We all do this, but I think it is more pronounced for trans people.” The blue and gold candle compact is “beautiful open or closed.” I was uncertain about the knife and wondered to myself if it was about “being under the knife” for his top surgery. Al clarified that, no, it was about the self-hate and when he was cutting. At the end of processing this sand tray Al looked at me and stated, “It’s taken a long time to be able to say I love myself…I’m glad I lived through it.” Momentarily overwhelmed by his affirmation, I managed not to tear up right there. As I later did my own processing of my work with Al, I realized that this type of outcome is why I continue to challenge myself to engage in deep therapeutic work.

For me as his older, cisgender female therapist, the difficult aspect of helping Al was not learning the language and the medical information of the transgender community. My greatest challenge was to maintain a life-to-life connection with him throughout his deep pain and despair. Holding Al’s anguish, self-hate, and constant self-deprecation, while providing him a glimmer of hope, took tremendous life force.
I hope that Al’s story will inspire you to expand your approach to help transgender youth. They are an underserved group requiring the competent and professional mental health care that you are capable of providing. Being transgender is not about sexual orientation—which is about who one loves. Being a transgender person is not a “choice” it’s about who one is. For Al it was an urgent, compelling need to become his authentic self. Al said it best, “I don’t want to be trans, nobody does.”
“Snapshots of Gender Transition” edited by Donna Parten, MSW (ret.).